Even though mental disorders are frequent, they are still being treated too late. The development of more accurate detection methods and new medications could change this for the better. In this respect, the contribution of research is crucial.
Our brain contains anywhere between 85 to 100 billion neurons. Each cell is connected to 10,000 others, meaning information can be exchanged up to 100 trillion times at once. This complicated and dynamic network can malfunction, leading to mental disorders such as Alzheimer’s disease, depression, and bipolar disorder.
These pathologies still occupy a special place in medicine, as explained by Jacques Gasser, head of the Department of Psychiatry at Lausanne University Hospital. Diagnosing these diseases remains a complex issue and always includes a certain degree of subjectivity. The latest medications cause fewer side effects, but still focus on suppressing symptoms instead of treating them. Finally, medicine cannot prevent the onset of these diseases.
This could all change thanks to the discovery of biomarkers that are specific to mental illnesses. A biomarker is a measurement of the signals generated by the various biological processes within the human body. This is the principle behind measuring a person’s cholesterol levels or blood pressure, foreboding signs of heart disease.
However, identifying biomarkers in an organ as complex as the brain is far from easy. Nevertheless, like neurobiologist Kim Do Cuénod, scientists believe finding them is crucial (read point 2). Biomarkers will make it easier to provide early treatment to people at risk of developing mental disease. They will also open the door to the development of objective diagnostic methods and new medications that are tailored to the needs of each patient.

Read our interview with Jacques Gasser

According to the Swiss Health Observatory, 18% of the Swiss population suffers from moderate to serious mental problems. Despite their frequency, these diseases are still being diagnosed too late. This is especially the case with psychosis. “Schizophrenia is often diagnosed two years after the onset of symptoms. A bipolar diagnosis can sometimes take up to 10 years,” explains Philippe Conus, head physician at the Lausanne University Hospital's General Psychiatry Service. “However, several studies have shown that the greater the delay between disease onset and the start of treatment, the poorer the patient outcome.”
Psychosis generally appears during the critical period of life at the end of adolescence and the start of adulthood.
For this reason, the Lausanne University Hospital launched the Treatment and Early Intervention in Psychosis Program (TIPP), which takes care each year of around 50 patients aged 18 to 35. This approach also raises ethical questions as society struggles to decide just how far these efforts should be allowed to go. “Our early intervention programme treats patients who are already showing clear signs of mental disease,” insists Philippe Conus. “The situation might be less clear with high-risk individuals, but these people are typically suffering from other issues, such as depression and anxiety, that require treatment. In this so-called prodromal phase, we use very low intervention strategies. At this point, we don’t prescribe neuroleptics and instead focus on psycho-social treatment.”

Read our interview with Philippe Conus
Early detection of mental disease also concerns the elderly population, observes Armin von Gunten, head of the University Service of Advanced Age Psychiatry (SUPAA) at the Lausanne University Hospital.
“People with a form of dementia such as Alzheimer’s disease also present with psychological disorders or behaviours, such as anxiety and depression. This often occurs at the early stage of the disease.”
These problems, which can include verbal and physical aggression, can quickly become problematic for both loved ones and healthcare staff. “Up until now, Alzheimer’s research hasn’t looked at this aspect of the disease, focusing instead on discovering treatments to modify how it progresses.”
That’s why Armin von Gunten and his team, in collaboration with the neurobiologist Ron Stoop, launched a study three years ago to identify the onset of these issues in patients suffering from the earliest stages of Alzheimer’s disease. One theory revolves around the role of ocytocin in forming personal attachments. “This hormone is a key factor in triggering uterine contractions during child birth and producing breast milk. It also influences the social ties between mother and child and, later on, between adults.”
The idea is that ocytocin could improve the personal relationships of patients with cognitive disorders. “The study was carried out using a translational approach. Ron Stoop’s team worked on animal models. Their results were then compared to a cohort of patients,” says Armin von Gunten. “The preliminary analyses support our hypothesis. If this is confirmed, the next step would be to decide how treatment could be adapted to the social attachment profile of each patient.”
Translational research is also the weapon of choice of Kim Do Cuénod, head of the Psychiatric Neurosciences Centre at CHUV, who has recently been awarded the 2018 Outstanding Basic Science Award by the Schizophrenia International Research Society (SIRS). For the past 15 years, the neurobiologist and her team have been collaborating with the psychiatrists at CHUV to better understand schizophrenia. “Up until now, neuroscience most often focused on basic research. The results of these studies were difficult to apply to humans,” says Philippe Conus. “With Kim Do Cuénod, we wanted to answer clinical questions by rounding out observations on human patients with findings in animal models and vice versa. The work is very circular in nature.”

Kim Do Cuénod, who has recently been awarded the 2018 Outstanding Basic Science Award by the Schizophrenia International Research Society (SIRS).
Their first study found that the brains of schizophrenic patients had a flawed antioxidant system. After characterising the mechanisms in experimental models, the Lausanne-based researchers teamed up with scientists from Harvard University to study the effects of N-acetylcysteine (NAC), a general antioxidant medication, on the early stages of psychosis. “The results are very promising,” says Kim Do Cuénod. “In order to treat patients early, we need biomarkers that can help us identify people who are at risk of developing the disease. We observed that NAC improves neuro-cognitive function in a subgroup of patients with a high level of oxidation in their blood.”
The study also shows that the medication improves structural and functional connections in the brains of these patients. The researchers then measured this progress using an electroencephalograph (editor’s note: an analytical method that measures the brain’s electrical activity). “These conclusions validate our strategy of using biomarkers to determine an appropriate treatment plan.”
The next step will consist of verifying the effects of NAC on a larger group of patients. “Our study involved a cohort of 60 people. We’ll need to confirm it with a much larger number of patients, which is very expensive. We’ll also need to identify more specific targets and treat them. As a result, our research is designed to be a long-term project. I also dedicate some of my time to fund raising, especially through the Alamaya foundation.”

In addition to establishing a partnership with neuroscientists over the past 15 years, psychiatric care professionals have also changed how they relate to patients’ family members. “Before, they were generally seen as contributing to the patient’s problems,” explains Roland Philippoz, head nurse and healthcare manager at the General Psychiatry Service at the Lausanne University Hospital.
“Looking at loved ones as partners and recognising their suffering and difficulties has been a significant change – one that didn’t come easily.”
What started as discussion groups at hospitals and outpatient clinics turned into support organisations for parents and loved ones of patients with psychotic, bipolar, or borderline personality disorders. “The underlying idea behind these efforts is to develop a community so people can reach out to each other and give voice to what they’re experiencing,” says Catherine Reymond-Wolfer, clinical nurse at the Lausanne University Hospital and committee member of L’îlot, a Lausanne-based association for the loved ones of patients with mental disorders.
Groups can also help rebuild bridges between the family and the healthcare staff. “Some mothers and fathers experienced physical or psychological violence from their child for months or years before seeking help. The situation became too much, and now they no longer want to hear from their offspring,” says Roland Philippoz. “It’s sometimes easier to understand the disease from the perspective of family members of other patients.”

Another major change took place this year in the form of a pilot project aimed at the children of people with mental disorders. The effort was launched by Christel Vaudan and Charlène Tripalo, a psychologist and a nurse in the Department of Psychiatry at CHUV. After creating a playroom where children could interact with their hospitalised parent and designating a representative to speak for the patients’ families, this initiative, called Famille+, focused on speaking with patients about parenthood. According to a recent study conducted in Winterthur, nearly 22% of people receiving treatment for a mental disorder have at least one minor child.
“Up until now, this question wasn’t asked systematically,” says Roland Philippoz. “The goal is not to think of these kids as being at risk and diagnosing them, but rather to address the suffering they’re experiencing due to the amorphous nature of their parent’s disease. That’s why we wanted to focus on the idea of parenthood in order to have discussions with the children – as much as the patients allow.”

Read Blaise Rochat's testimony
Healthcare professionals quickly come up against the limits of doctor-patient confidentiality. In fact, it’s one of the topics highlighted through a series of events organised this year by the General Psychiatry Service. “On the one hand, patients often don’t want us to talk about their case, but on the other hand, families complain about being kept out of the loop. Establishing a constructive relationship without talking about important questions is very difficult. Being able to negotiate with the patient is critical to finding a solution to this impasse.”
The event’s awareness-raising efforts are mostly aimed at staff. In the service, the average age on the teams is 29; most employees haven’t had children yet. “We want to promote an intergenerational perspective so parents aren’t stigmatised as ‘those people who make us crazy,’” says Roland Philippoz. “When you’re a parent yourself, you have a better understanding of the difficulties experienced by someone who’s the cause of so many challenges and the resources needed to support them.”
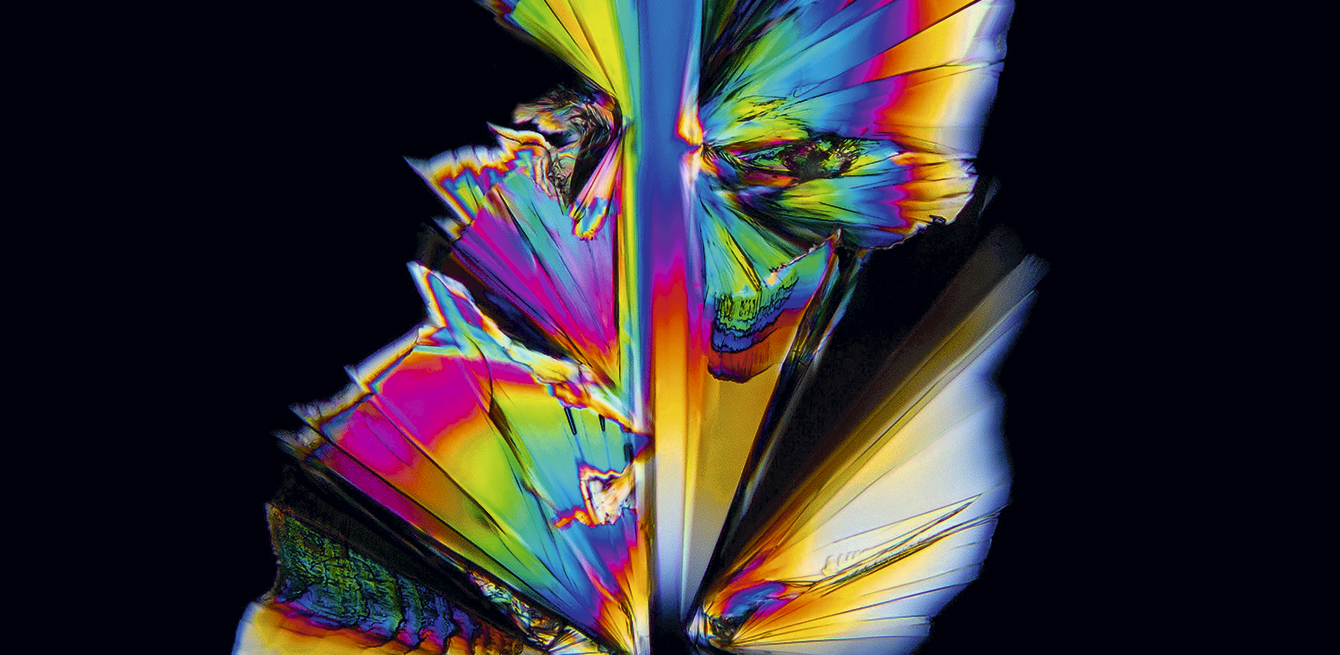
Better known by its commercial name Prozac, this substance discovered in 1974 is used in the treatment of depression.
Zoom on four research projects carried out within the Department of Psychiatry at the Lausanne University Hospital.





The number of people affected by mental disorders in Switzerland.
/
The percentage of young people suffering from mental illnesses.
/
Number of research axes within the Department of Psychiatry at CHUV: neuroscience, psychotherapy, human sciences, public health and epidemiology.
As far back as Hippocrates, medicine has sought a cure for depression, which the famous physician of ancient Greece referred to as melancholy. This disease is associated with both physical and psychological symptoms, including unusual fatigue, trouble sleeping, lack of appetite, low libido, constant feelings of sadness or negative thoughts, and the loss of self-esteem. Now more than ever, depression is a major public health problem. Estimates put the cost of the disease in Switzerland at over 10 billion Swiss francs per year. Nearly 25% of the Swiss population will suffer from severe depression at least once in their lifetime.
Often incorrectly used to refer to multiple personality disorder, the term schizophrenia comes from two ancient Greek words: skhizein (break) and phren (thought). This mental disorder typically appears in young adulthood. Initial symptoms include a withdrawal from society and a break with reality. In the acute stage, this type of psychosis triggers auditory hallucinations that can be highly disturbing for the patient. A multitude of factors contribute to the appearance of schizophrenia, including social, psychological, and genetic aspects. Nevertheless, medicine does not yet fully understand the causes of the disease, making it sometimes difficult to establish a precise diagnosis.
People living with bipolar disorder experience cyclical patterns of intense euphoria and profound depression. In 1899, the German doctor Emil Kraepelin was the first to describe the modern conception of this disease, which was once called manic-depressive psychosis. During the depressive phase, patients feel sad and tired and are uninterested in the activities of day-to-day life. Conversely, during the manic phase of the disease, patients are full of energy and talkative, jumping from one subject to the next. They can also experience delusions and hallucinations.
Personality disorders include a wide range of maladaptive personality patterns. They can affect an individual’s cognition, feelings, or interpersonal relationships and cause suffering or impede his or her ability to function in society. The fifth edition of the Diagnostic and Statistical Manual of Mental Disorders, the last word in psychiatry, identifies three major categories: eccentric disorders; dramatic, emotional, and erratic disorders; and anxious and fearful disorders.
The image most often associated with obsessive-compulsive disorder (OCD) is that of a person who washes their hands repeatedly. OCD is a type of anxiety disorder characterised by recurrent (obsessive) thoughts that the individual tries to relieve through specific rituals (compulsions). Affecting equal numbers of men and women and first appearing during both childhood and adulthood, OCD is the fourth most common mental disorder in the world. Because obsessive-compulsive disorder has a neurological component, it can be triggered by an infection of the central nervous system, such as encephalitis. Other neuro-degenerative diseases can also be associated with the onset of this pathology.