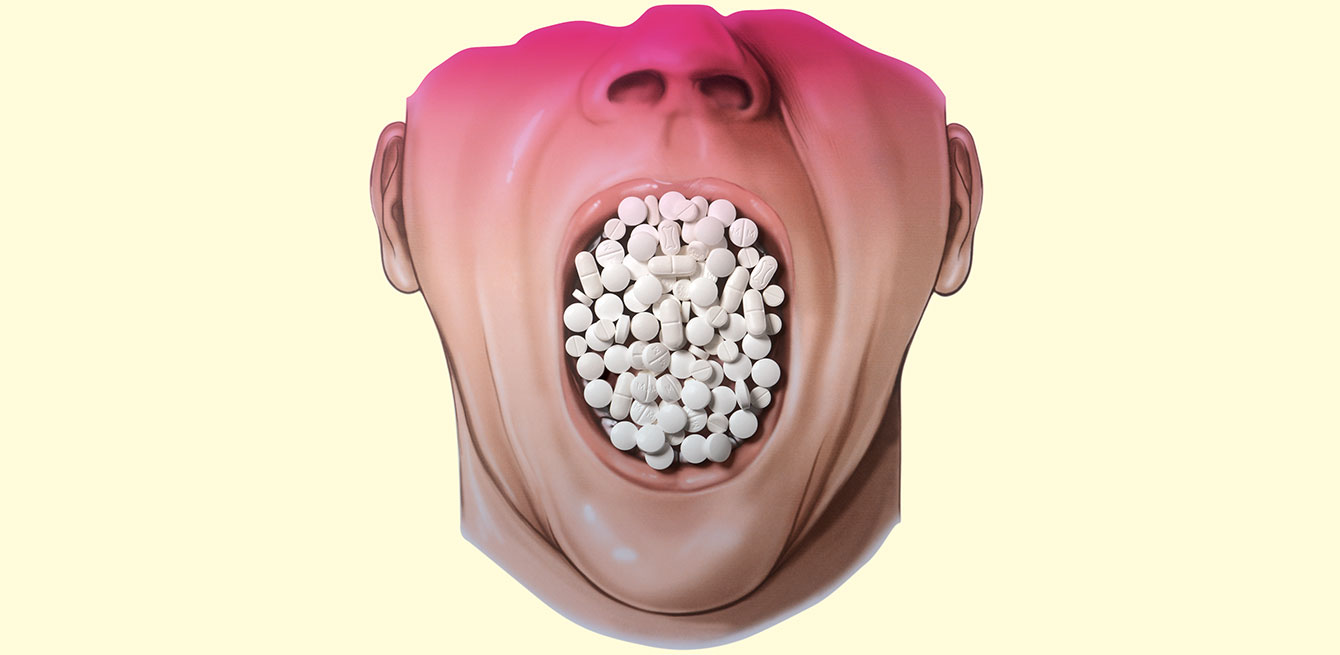
People are beginning to speak out against over-medicalisation. measures are being taken to encourage less care, even if that means giving up old certainties.
www. smartermedicine.ch this swiss platform designed for patients and specialists provides an updated list of procedures deemed unnecessary, available in german and French.
www.lessismoremedicine.com this website includes press articles, events and blog posts about over-medicalisation (in english and French).
www.choosingwisely.org the US campaign choosing wisely promotes dialogue between patients and health- care professionals about the treatments they are offered (in english).
Are our modern doctors all dr Knock? this fictional character dreamt up by the French writer Jules romains in the 1920s convinced the in- habitants of an entire village that they were ill and had to be treated. similar to molière with his Imaginary Invalid, romains criticised the excesses of an overmedicalised society that transforms citizens into health care consumers who just keep wanting more, hoping to feel better and better.
over-medicalisation has been around for decades. But in the 21st century, health care is no longer reduced to bleeding, purging and other old-fashioned remedies. a growing number of increasingly sophisticated high-tech instruments and drugs give doctors an ever greater arsenal of therapies to choose from.
“When a new product is released on the market and its manufacturers extol its virtues, as physicians, we want to believe it,” says thomas Bischoff, director of the Institute of Primary Care at the University of Lausanne.
“While maintaining an analytical perspective, we hope that it will truly help us provide better care for our patients. but it’s not easy for the medical community to separate the good from the bad with all these new products.”
Patients also hope that new cutting-edge technology or treatments will cure them. and the healthy are advised to remain prudent. “patients are constantly bombarded by warnings coming from public health campaigns, media and advertising to get screened or treated,” says rosemary gibson, author of The Treatment Trap. “their belief that ‘prevention is better than cure’ runs deep.”
David Goodman, professor of community medicine at the university of bern, notes that “early detection and aggressive treatment are often considered evidence of quality care.”
Patients and health care professionals firmly believe in the promises of modern medicine. even though dr Knock ends up winning in the play by Jules romains, a growing number of health care providers today instead support more humble, modest form of medicine that recognises its limitations and is bold enough, in some cases, to do less.
“We’re seeing movements emerging that advocate the idea of ‘less is more’ in medicine,” says Arnaud Chiolero, public health specialist at the university institute of social and preventive medicine in lausanne.
“The objective is especially to perform fewer unnecessary treatments.”
Campaigns like smarter medicine in Switzerland, or choosing Wisely and slow medicine in the
united states, are embracing medical care that is moderate and gradual. doing less in no way means questioning necessary and useful treatments for patients. the “less is more” concept invites people to acknowledge that too much medical treatment can sometimes be more risky than beneficial.
Proponents believe that Western societies are currently over-medicalised. “We’re in a health care system that constantly pushes us towards ‘excessive’treatment,” says Thomas Bischoff. “that can be explained by the same principle that encourages other sectors in our Western cultures to keep going further. We view accumulation and growth as signs of progress and performance.”
Full-time Patient
This general practitioner believes that medicine takes up too much of people’s lives today. “We don’t just go to the doctor when we’re sick, we also have routine checks and other tests done,” he notes. “and that can transform healthy people into potential patients.”
Outside medical offices and hospitals, some people constantly focus on monitoring their health.
“With new technology, applications and connected objects, anyone can measure their insulin levels, pulse or blood pressure whenever they want.”
If they find anything suspicious, the temptation is nearly irresistible to seek out more information online. according to a study published by swisscom in 2012, 84% of swiss people have already done research on medical websites before or after seeing a doctor. the most common searches are about symptoms, diseases and possible treatments. “patients feel reassured when they leave with a prescription,” says Peter Vollenweider, chief physician at the service of internal medicine at Lausanne university hospital (CHUV). “prescribing medication takes up less of a doctor’s time than explaining why not to. but we need to take that time if we believe that the treatment has nothing positive to offer the person in front of us.”
Quand la pilule s’efface face au relationnel
En psychiatrie, les traitements médicamenteux peuvent être complétés par des thérapies relationnelles. «L’art-thérapie, la musico-thérapie ou l’ergothérapie appartiennent à une palette de prestations qui peuvent être activées en fonction des besoins du patient, relève Jean-Michel Kaision, le directeur des soins du Département de psychiatrie du CHUV. Certaines activités de la vie quotidienne, comme la promenade ou la lecture, en font aussi partie.» Le but ici est de séquencer et d’organiser la journée du patient pour lui permettre de retrouver des repères. «Des études récentes ont démontré que ces thérapies sont efficaces également chez les personnes âgées atteintes de démence ou d’Alzheimer», précise le spécialiste.
Il n’est pas rare qu’elles permettent de réduire la consommation médicamenteuse du patient. Les personnes souffrant de troubles du sommeil sont par exemple traitées au moyen de massages ou du Snoezelen, une technique néerlandaise qui consiste à placer le malade dans une pièce spécialement équipée pour stimuler tous ses sens au moyen de musique, lumières colorées, odeurs relaxantes et matelas composés de différents matériaux. «Cela permet de calmer le patient pour qu’il arrive plus détendu dans son lit», détaille Jean-Michel Kaision.
On se rend alors souvent compte qu’il n’a plus besoin du somnifère qui lui est normalement administré.
Senior citizens on the front line
This issue is especially prevalent among the constantly growing elderly population, who are huge consumers of medication. a 2013 study by the French society of geriatrics and gerontology reported that more than 90% of people over age 80 took an average of ten pills a day. the coordinator of the study, Olivier Saint-Jean, chief of the department of geriatrics at Georges Pompidou european hospital in paris, said in an interview with the French newspaper Libération, “any more than three or four molecules taken together and we don’t know how they will react. and, more importantly, beyond five, the risk of a medication accident increases considerably.”
the French may be some of the world’s biggest consumers of medication (see infographic on the right), but the numbers are also high throughout the rest of Europe. a survey published by the swiss paper L’Hebdo in April 2015 reported that nearly 20% of patients age 80 and over took ten types of medication or more per day, and 50% to 60% took at least five.
“each additional drug increases the chances of experiencing a side effect or triggering an interaction with another compound,” says Robert Vander Stichele, professor of clinical pharmacology at the university of ghent (Belgium) and author of several studies on the consumption of medication by senior citizens. When diabetes medication is given to someone whose blood sugar level is barely above average, they risk going into hypoglycaemia and falling or losing consciousness, especially if the person is elderly.
Technological advances can now detect abnormalities in their early stages that used to be invisible.
That all looks good on the surface... “diagnostic tests have become more sensitive,” says Arnaud Chiolero. “For example, ct scans are used to identify pulmonary emboli that are merely harmless mini-emboli.” similarly, a routine X-ray procedure can often reveal a spot on the kidney, a lump in the breast or a nodule in the lung that could be cancerous lesions, but for the most part are innocuous.
Once the abnormality has been identified, “it’s virtually impossible, even unethical, not to investigate further and treat the patient, even if that means a high likelihood of over-diagnosis,” says the Lausanne-based physician in a research paper.
“doctors also fear regretting not having anticipated more, once the cancer is reported,” says Jacques Cornuz, director of the lausanne university medical polyclinic. “how can we be sure that a lesion is harmless? screening always looks more attractive than it actually is, for both doctors and patients.”
Raising Awareness Among young doctors
medical students have not been adequately exposed to the issue throughout their training. “as physicians, we are taught to act, not to remain passive when dealing with illness,” says David Goodman. “modern medicine is based on action,” adds Gian Domenico Borasio, professor and chair in palliative medicine at the university of lausanne and chief of the palliative care service at the CHUV.
“We now need to set off a change in culture by encouraging young physicians to get out of that trap of taking action at any cost.”
Economic interest
some procedures are overused for economic reasons, such as implanting certain stents – those small prosthetic devices used to widen blocked blood vessels. in Switzerland, they doubled in number between 2002 and 2013, going from 11,000 to 22,000. this rise is partly due to population ageing and the fact that this treatment is now frequently offered to patients over 80, explained Urs Kaufmann, president of the swiss society of cardiology, in an April interview published in Le Matin Dimanche and SonntagsZeitung. “but this increase also suggests that the patient’s well-being is not always the main reason for initiating the procedure,” he says. “these procedures are lucrative and easy to plan. We might suspect that some hospitals place purely financial considerations before medicine.”
Arnaud Chiolero adds, “a growing number of stents are implanted, while a more conservative treatment based on medication and a change in lifestyle [editor’s note: quitting smoking, losing weight] would often be enough.”
it is high time to find solutions to remedy the problem of overmedicalisation. general practitioners have a crucial role to play. “the family doctor must consider the patient as a whole,” says Thomas Bischoff. “specialists prescribe treatments to deal with a specific condition, but a patient with several conditions will be taking multiple treatments at the same time,” he goes on. “the general practitioner should be able to prioritise treatments and find a balance that the patient can tolerate.”
Separating the good from the bad
In 2000, Sweden defined a “Wise list”. this list, established by an independent scientific committee, includes the 200 essential drugs for treating common diseases. in 2012, 90% of the prescriptions written in stockholm were compliant. France plans to define a similar list by 2016. a preliminary document lists 151 drugs out of more than 5,000 on the market.
“in Switzerland, each hospital prepares its own list of essential drugs,” says Pierre Voirol, head pharmacist at the pharmaceutical assistance and clinical pharmacology unit at the CHUV. “ours includes 1,000 drugs out of the 2,200 in stock at the hospital.” What gets a drug on the list? “its effectiveness, tolerance by patients and variety of forms available [editor’s note: tablet, liquid, powder, etc.]. cost is only factored in as a secondary criterion.”
Pierre Voirol also coordinates a drug commission to issue recommendations to prevent duplicating treatments and prescribing unnecessary ones. he points to benzodiazepines – often prescribed twice to treat both insomnia and anxiety – while one would be adequate. he also notes that, instead of administering antibiotics intravenously, it would be safer for the patient and less costly to take them orally once the patient is stabilised. “if a new medication hits the market, we will also specify in which cases it’s worth using it and when an existing treatment should be used,” he adds.
pharmacists from Pierre Voirol’s unit are also in charge of assisting doctors during their patient rounds to examine their medication and make recommendations. “For example, we’ll remind them that administering a drug against stomach ulcers is not necessarily required after the patient is released from intensive care.” this process would be simplified even further with the more standardised use of electronic patient health records. “all those data grouped into one place,” he says, beaming.
More honest medicine
in many countries, doctors’ organisations have taken steps to set out guidelines that would reduce the prescription of unnecessary exams or drugs with little or no value. on request from the swiss society of general internal medicine (sgim),
Jacques Cornuz laid out a list of avoidable procedures. “certain exams and treatments are used, but no one really knows if they offer any significant improvement to the patient’s health,” the physician says. “When clinical and epidemiological research confirms the lack of any beneficial impact, medicine should be honest enough to acknowledge it.”
At the end of 2014, the SGIM singled out five common procedures as “unnecessary” in Switzerland (www.smartermedicine.ch). its “top 5” include Xrays to investigate certain types of lower back pain, antibiotics for bronchitis and other infections of the upper respiratory tract, X-rays before certain operations and proton pump inhibitors to treat stomach acid. in the united states, a similar list covers about fifty guidelines (see p. 25). the swiss list may eventually incorporate other procedures.
One of these is testing prostate specific antigen (psa) levels in the blood to detect prostate cancer. patients should be provided with neutral information about the advantages and disadvantages of the test before having the procedure performed, which the sgim does not recommend for men over age 75. “many cancerous lesions found in patients without any symptoms will never develop into the disease, at least not during their life time,” says Arnaud Chiolero.
Peter Vollenweider adds that high psa levels do not necessarily mean that the patient has cancer, “but they lead us to run other tests, which can increase the burden and stress put on patients. if cancer is actually reported, they could undergo an operation that will affect their sex lives and sometimes social lives but without necessarily increasing their life expectancy,” he explains. “is the treatment really worth it? the decision must not be made by the doctor alone. the patient needs to understand all sides of the issue and give an opinion.”
Patient care Plans
Involving patients more in decisions about their treatment is one of the highly recommended measures taken to reduce the overuse of medical services. “patients should be presented with the pros and cons of each option, so that they can make well-informed choices,” says Jessica Otte, a Canadian family physician who created the health care blog less is more. a study by the group health research institute in Seattle demonstrated that when patients were provided with decision aids in the form of informational videos, 38% of them opted against knee surgery, while 26% refused a hip replacement.
Working with patients and their family is even more important in the case of a chronic and progressive disease. “it is vital that we discuss their values and priorities early on in their treatment,” says Gian Domenico Borasio. “do they prefer to be treated at home? in a facility? What are their fears? What are they definitely against? addressing these issues early helps set out a patient care plan in line with their personality and preferences.”
The specialist points out that since October 2014 all medical students at the university of lausanne now take both a clinical and classroom course on palliative care. “in some situations, it can be very beneficial for the patient. the treatments given do not try to extend the patient’s life but improve its quality,” he says. “one unexpected finding of various studies is that palliative care can also extend the person’s life, while making their day-to-day existence more comfortable. that’s why i think that each clinician should have some basic knowledge about palliative medicine to talk about it with their patients suffering from one or more
chronic and progressive diseases.”
Gian Domenico Borasio believes that the danish philosopher Søren Kierkegaard perfectly expressed the attitude that doctors should have in their day-to-day practice: “if one is truly to succeed in leading a person to a specific place, one must first and foremost take care to find him where he is and begin there. this is the secret in the entire art of helping. anyone who cannot do this is himself under a delusion if he thinks he is able to help someone else.” and he concludes, “to guide patients well, we must first understand and respect their priorities. at no point should we ever abandon a person, but sometimes we need to know when to abstain for their benefit.” /
People who take the most medication do not necessarily live longer.
is the annual cost of excess health care worldwide, estimated by the Dartmouth Institute.
is the percentage of unnecessary
drugs, of which 5% are potentially
harmful, according to The Guide
of 4,000 Useful, Unnecessary or
Dangerous Drugs (Le Guide des
4000 médicaments utiles, inutiles ou
dangereux), published by a surgeon
and a French pulmonologist.
Remember back in september of 2004 when the pharmaceutical group merck recalled its blockbuster vioxx, the anti-inflammatory painkiller drug that used to generate two billion dollars a year in revenue?
Why?
The drug, commonly prescribed to arthritis patients, increased the risk of heart attacks and strokes, causing more than 30,000 deaths in the united states alone.
Another health scandal exploded a few years later.
This time it involved mediator, a drug developed by servier laboratories and sold as an anti-diabetic.
From its market launch in 1976 until its recall in 2009, 145 million boxes were sold, and more than 5 million people had taken the drug in France.
According to the inspection report published in 2013, from the university of Bern, the drug caused damage to heart valves and a form of pulmonary hypertension, killing nearly 2,000 people.
These two highly publicised cases, along with the explosion of health care costs starting in the 1990s, thrust the issue of over-treatment into the spotlight.
Opinions started to sway in favour of fighting this trend. “the movement began in the United-States. Europe didn’t join in until later, probably because health care costs are not as excessive, and the need to stabilise them less urgent,” says David Goodman, from the University of Bern.
The issue is not unique to modern societies. “back in the 18th century, doctors complained that their patients were only satisfied if they left with a remedy in hand,” says micheline Louis-Courvoisier, a medical historian from the University of Geneva. in some ways, the situation was even worse than it is today, as the medical field was more open in those days, with healers and bonesetters providing treatments in the same way doctors did. “it wasn’t until the 19th century that doctors and surgeons teamed up to form guilds, relegating other types of healers to society’s margins.”
In some ways, the situation was even worse than it is today, as the medical field was more open in those days, with healers and bonesetters providing treatments in the same way doctors did. “it wasn’t until the 19th century that doctors and surgeons teamed up to form guilds, relegating other types of healers to society’s margins.”
The american researcher John wennberg’s work in the 1970s considerably raised people’s awareness about over-medicalisation. He demonstrated that 7% of children from middlebury, vermont, had their tonsils removed, compared with 70% in stowe, 80 km away. this “unwarranted variation” could not be explained by any other reason than the fact that some doctors are a bit overzealous with the knife.
Created by about fifty US medical organisations, the Choosing Wisely list covers tests and procedures that can be avoided.
Some of the examples include:
Only 0.5% to 2% of cases of sinusitis develop into a bacterial infection. antibiotics should therefore be avoided for moderate symptoms that clear up on their own within two weeks. the same applies for ear infections.
Each transfusion bears risks, especially of allergic reactions. a limited amount of blood (7 to 8 g/dl) is enough for stable patients. anaemics should be treated with oral supplements rather than transfusions.
Pap smears are ineffective in detecting cervical cancer in women under 21. most abnormalities that occur at this age clear up on their own. in women age 30 to 65, a test every three years is adequate.
Prescribing antipsychotic drugs and sleeping pills to older patients with dementia should be a last resort to be used only after other non-medical treatments have failed. these medications increase the risk of stroke, falls and premature death.
Metastatic breast cancer should be treated with only one chemotherapy drug instead of combining several. the second option does not increase the chances of survival, but has more severe side effects.
Non-invasive treatments (physical exercise, anti-inflam- matory drugs, mild painkillers or cortisone shots) are more effective than arthroscopic knee surgery.